Despite widespread acceptance that most psychiatric disorders are "diseases of the brain" (1), the field of psychiatry has thus far failed to identify a single neurobiological marker that is diagnostic of a mental disorder (2). There are a number of potential advantages to including laboratory tests in diagnostic criteria. In contrast to the clinical signs and symptoms that form the basis for the current DSM criteria, laboratory tests are more objective (3), would facilitate detection of mental disorders in primary care settings (4), and would highlight the neurobiological basis of psychiatric disorders.
Friday, December 22, 2006
Including Laboratory Tests in DSM-V Diagnostic Criteria
Friday, December 15, 2006
Friday, December 08, 2006
Some recent publications ...
DSM and the Death of Phenomenology in America: An Example of Unintended Consequences.
Nancy C. Andreasen, Schizophrenia Bulletin, doi:10.1093/schbul/sbl054.
The Search for New Off-Label Indications for Antidepressant, Antianxiety, Antipsychotic and Anticonvulsant Drugs.
Guy Chouinard, M.D., Focus 4:528, September 2006.
Middle and Inferior Temporal Gyrus Gray Matter Volume Abnormalities in First-Episode Schizophrenia: An MRI Study.
Noriomi Kuroki, M.D., et al., American Journal of Psychiatry 163:2103-2110, December 2006.
What Is Familial About Familial Bipolar Disorder? Resemblance Among Relatives Across a Broad Spectrum of Phenotypic Characteristics.
Thomas G. Schulze, M.D., et al., Archives of General Psychiatry, 2006; 63:1368-1376.
Practice Guidelines for the Treatment of Psychiatric Disorders: Compendium 2006.
American Psychiatric Association.
Postpartum Depression: A Major Public Health Problem.
Katherine L. Wisner, MD, MS; Christina Chambers, PhD, MPH; Dorothy K. Y. Sit, MD, Journal of the American Medical Association, 2006; 296:2616-2618.
Modeling Sensitization to Stimulants in Humans: An [11C]Raclopride/Positron Emission Tomography Study in Healthy Men.
Isabelle Boileau, PhD, et al., Archives of General Psychiatry, 2006; 63:1386-1395.
Saturday, December 02, 2006
Nicotine Receptor Agonist Could Aid Smoking Cessation
Counseling, CBT, and nicotine patches can help schizophrenia patients who want to quit smoking. However, other interventions — such as a nicotinic receptor agonist called DMXB-A — may work even better.
References:
Am J Psychiatry 163:1934-1942, November 2006
Am J Psychiatry 163:11, November 2006
Friday, December 01, 2006
Wednesday, November 29, 2006
Dr. Paul Greengard on Depression
Every year, without any treatment at all, thousands stop suffering from depression. Because it kills them.
Mental Health Bill 2006 (United Kingdom)
The Mental Health Bill 2006 amends the Mental Health Act 1983. It also introduces "Bournewood" safeguards through amending the Mental Capacity Act 2005. The Bill was introduced into Parliament on 16 November 2006.
Sunday, November 26, 2006
FAQ on Mental Illness and Mental Health
Friday, November 24, 2006
Fine Line: Mental Health/Mental Illness
 From the website:
From the website:FINE LINE is a documentary of voices, stories and portraits that confronts stereotypes and reveals the courage and fragility of those living with mental illnesses.
Photographer Michael Nye spent four years photographing and recording stories. Schizophrenia, depression, obsessive-compulsive, anxiety and bi-polar disorders are among the experiences considered.
In simple and eloquent detail the 55 black-and-white portraits and voices draw you closer into each life by addressing and exploring many topics: family, confusion, pain, abuse, treatment and healing.
Consider Beth. She was one of the most talented writers in her high school – she performed her own original songs on stage. Later, she was unable to leave her home, and literally stayed in one chair in her kitchen for years.
Thelma raised six children on the banks of the San Antonio River and sings Mexican ballads when she’s alone. When she was 10, her mother tried to crash a hired plane in the desert with her on board.
At the age of 20, Kerry built a house that was featured on the cover of an architectural magazine. At the age of 49, he hung himself in his mother’s garage. He was gentle, kind, intelligent and shy.
Doris received a Master’s Degree in sociology. Her passion is collecting recipes. She was homeless for 2 years. As a child she was beaten and sexually abused.
Michael was the editor/part owner of an alternative newspaper. His gift is making people laugh. He had his first breakdown at the computer screen. He started crying for no apparent reason and could not stop.
Deeply personal stories can take us inside complicated issues where empathy and understanding begin. Each face invites you to listen.
Anxiety and Happiness
Thursday, November 23, 2006
Human Genome more Variable than Previously Thought
"We have to think of genetics in an entirely different way. We're actually more like a patchwork of genetic code than bar codes that line up evenly," Dr. Scherer said. "Everything we've been taught is different now."The study, conducted by Canadian, British, American, and Japanese researchers, was published today by the journal Nature. It also made headlines in The Times Online (where it is accompanied with a nice explanatory graphic).
Also see:
CBC News
BBC News
National Geographic News

Photo caption from National Geographic News:
A new DNA study has revealed that humans show much more genetic variation than was previously believed. Scientists studying how large chunks of DNA differ among individuals found large changes in 12 percent of the human genome.
Here, superimposed profiles of different human genomes reveal the magnitude of differences, with green segments showing DNA gains, red areas representing losses, and yellow portions indicating no difference.
Image courtesy Matthew Hurles/Nature
Tuesday, November 21, 2006
Atomic-level Scrutiny of Neurotransmitter Vesicles is a First
The first depiction of an organelle right down to its molecular minutia has finally come to light. Using a combination of biophysical and proteomic techniques, European and Japanese scientists examined quantitatively the relative ratios of the lipids and 180 or so proteins that adorn synaptic vesicles, the compartments that house and traffic neurotransmitters essential for brain function (Cell 2006, 127, 671).
This picture of a synaptic vesicle is the first atomic-level description of any cellular organelle. Cell © 2006
Next up, the researchers will focus on how vesicles that carry different neurotransmitters — such as glutamate or gamma-aminobutyric acid — differ from one another.
Thursday, November 16, 2006
Violence and Mental Illness — How Strong Is the Link?
"The challenge for medical practitioners is to remain aware that some of their psychiatric patients do in fact pose a small risk of violence, while not losing sight of the larger perspective — that most people who are violent are not mentally ill, and most people who are mentally ill are not violent."He also noted:
"A study that compared the prevalence of violence in a group of psychiatric patients during the year after hospital discharge with the rate in the community in which the patients lived showed no difference in the risk of violence between treated patients and people without a psychiatric disorder. Thus, symptoms of psychiatric illness, rather than the diagnosis itself, appear to confer the risk of violent behavior."An interview with Dr. Friedman can be heard by clicking here.
Wednesday, November 15, 2006
This Man has a Problem
Thanks to Liz Spikol for bringing this video to my attention.

"Functional MRI, recent advances in genetics, and improved understanding of neurophysiology are all contributing to a better understanding of how brain function influences mind, and how mind, meaning and experience can change the brain."A conference well worth attending?
Monday, November 13, 2006
Shared Decision Making and Medication Management in the Recovery Process
In the recent issue of Psychiatric Services, Patricia E. Deegan, Ph.D. and Robert E. Drake, M.D., Ph.D., have published an interesting article.
Here is the abstract:
"Mental health professionals commonly conceptualize medication management for people with severe mental illness in terms of strategies to increase compliance or adherence. The authors argue that compliance is an inadequate construct because it fails to capture the dynamic complexity of autonomous clients who must navigate decisional conflicts in learning to manage disorders over the course of years or decades. Compliance is rooted in medical paternalism and is at odds with principles of person-centered care and evidence-based medicine. Using medication is an active process that involves complex decision making and a chance to work through decisional conflicts. It requires a partnership between two experts: the client and the practitioner. Shared decision making provides a model for them to assess a treatment's advantages and disadvantages within the context of recovering a life after a diagnosis of a major mental disorder."
Sunday, November 12, 2006
Troubled Children
"At a time when increasing numbers of children are being treated for psychiatric problems, naming those problems remains more an art than a science. Doctors often disagree about what is wrong.[ ... ]
But there are also deep uncertainties in the field itself. Psychiatrists have no blood tests or brain scans to diagnose mental disorders. They have to make judgments, based on interviews and checklists of symptoms. And unlike most adults, young children are often unable or unwilling to talk about their symptoms, leaving doctors to rely on observation and information from parents and teachers."
Saturday, November 11, 2006
CAMH Publishes Important Study on Depression

The next step for researchers will be to investigate why MAO-A levels are raised in the brain and to consider prevention strategies.
Friday, November 10, 2006
Healthy Minds Initiative: Update to the Community
Criterion 10: We espouse a core set of Values & Principles that guide everything we do.
Our Values are:
- People First
- Responsibility To The Community
- Whatever We Do Is Based On Evidence
Our Principles are:
We espouse to:
- Share responsibility - every person is responsible to contribute to his or her own health and to that of our community.
- Meaningfully exercise (role model) our responsibility for our own health and that of our community.
- Build capacity to contribute, partner and create meaning as healthy citizens living in our community.
- Work with both health and illness.
- Build a coalition that is a resource to individuals and the community. This coalition will be jointly accountable with the community, building capacity within our ability to sponsor health, treat illness and support recovery.
- Value all forms of human knowledge and experience - individual and communal; subjective and objective - and recognize that human understanding can spring from intuition or from empirical evidence.
- Evaluate what we do and demonstrate it to be effective.
Thursday, November 09, 2006
Religion and Spirituality
"Although more clinicians are considering patients' religion and spirituality in their initial evaluation than in the past, these issues may need to be revisited at various times during psychiatric treatment."
"A study in the September Canadian Journal of Psychiatry adds a new twist to the question of whether religiousness affects people's emotional states. It has linked religiousness with lower rates of both depression and anxiety, yet has found that spirituality — the search for a meaning to life — is associated with higher rates of both maladies."
Bipolar psychopharmacotherapy – caring for the patient
Bipolar psychopharmacotherapy – caring for the patient
By Hagop S. Akiskal and Mauricio Tohen (eds), Wiley & Sons Ltd, 30 November 2005, 399pp, ISBN 139780470856079 (HB), Price CDN $116.99
Send me an email if you are interested in more information.
Wednesday, November 08, 2006
Chronic stress affects attention by altering neuronal growth in the brain
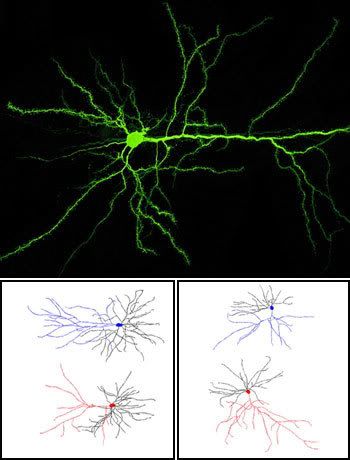 Branching out. Unlike a typical rat neuron (top), the growth of neurons in stressed rats can be impacted by traumatic experiences. Computer models based on McEwen's experiments (bottom) show that when compared to neurons of unstressed rats (blue), neurons from stressed rats (red) often develop either fewer dendritic branches or more, depending on their location in the brain
Branching out. Unlike a typical rat neuron (top), the growth of neurons in stressed rats can be impacted by traumatic experiences. Computer models based on McEwen's experiments (bottom) show that when compared to neurons of unstressed rats (blue), neurons from stressed rats (red) often develop either fewer dendritic branches or more, depending on their location in the brain "One of the characteristic manifestations of prolonged stress is decreased performance in tasks that require attention, including the ability to shift focus as well as to learn and unlearn information," notes a recent press release from Rockefeller University.
"Bruce McEwen, Rockefeller’s Alfred E. Mirsky Professor and head of the Harold and Margaret Milliken Hatch Laboratory of Neuroendocrinology, was interested in finding out how this translates to changes in the brain itself. So he and Conor Liston, a graduate student in McEwen’s lab, compared neuronal change in stressed and unstressed rats."
"Working neuron by neuron, researchers have found that life experiences actually appear to change the length and complexity of individual brain cells ... chronic daily stress affected neurons in two different areas of the rat brain, showing for the first time a link between anxiety symptoms and the dynamic anatomy of the brain."
Thanks go to Nutmeg for alerting me to this Journal of Neuroscience article.
Sunday, November 05, 2006
Psychotherapy Innovator Wins Research Award
"Cognitive enhancement therapy that seeks to teach discrete social and neurocognitive abilities to patients with schizophrenia is the newest wrinkle in an evolving field of psychosocial treatment pioneered by Gerard Hogarty, M.S.W. Hogarty died at age 70 on April 7, 2006."
"Hogarty, a professor emeritus of psychiatry at the University of Pittsburgh School of Medicine, was posthumously awarded the APA/American Psychiatric Foundation Alexander Gralnick, M.D., Award for Research in Schizophrenia at the 58th Institute on Psychiatric Services last month."
Saturday, November 04, 2006
Margaret Trudeau's Triumph
Wednesday, November 01, 2006
Evening Hours Now Available
If you would like an evening appointment, please contact one of the Community Mental Health Teams listed below:
Bedford-Sackville Team: (902) 865-3663
Dartmouth City Team: (902) 464-3116
Halifax Abbie Lane Team: (902) 473-2531
Cole Harbour / Eastern HRM Team: (902) 434-3263
Hants Community Team: (902) 792-2042
Sunday, October 29, 2006
Food Assistance in Halifax Regional Municipality
Brunswick Street United Church, 2107 Brunswick Street, Halifax (Breakfast, Monday through Friday, 7-8 am): (902) 423-4605 or (902) 423-2107
Feed Nova Scotia (Food and Assistance): (902) 457-1900
Feeding Others of Dartmouth, 43 Wentworth Street, Dartmouth (Lunch: Everyday, Noon to 12:30 pm; Supper: Monday, Tuesday, and Wednesday, 4:30 pm to 5:00 pm): (902) 464-2919
Hope Cottage, 2435 Brunswick Street, Halifax (Meals, Monday through Friday, 10 am to 11 am and 5 pm to 6 pm): (902) 429-7968
Saint Andrew’s United Church, 6036 Coburg Road, Halifax (Supper, Sundays, 4 pm to 6 pm): (902) 492-1454
Saint George’s Anglican Church, 2222 Brunswick Street, Halifax (Supper, Saturdays, 4 pm to 6 pm): (902) 423-1059
Saint Matthew’s United Church, 1479 Barrington Street, Halifax (Breakfast, Sundays, 9 am to 10 am): (902) 423-9209
Society of Saint Vincent de Paul (Assistance): (902) 422-2049 or (902) 466-6183
St. Paul’s Food Bank, Spryfield (Food): (902) 479-1015
Note: An excellent listing of food banks and related agencies in Nova Scotia can be found here.
Wednesday, October 25, 2006
Open Groups, Mental Health Outpatient Department, Halifax
Note: Sometimes a group might be cancelled due to unforeseen and/or unplanned circumstances. Every attempt will be made to notify people of any cancellations one week prior to the next group. However, if you are planning to attend a group for the first time, please contact the Mental Health Outpatient Department to confirm that the group is being offered. The phone number is (902) 473-2531.
For more information on a specific group, click on the applicable heading.
Self-Esteem
Wednesdays: 1:30 pm to 3:00 pm
Mental Health Outpatient Department Conference Room #3032, 3rd Floor
QEII Heath Sciences Centre
Abbie J. Lane Building
5909 Veterans’ Memorial Drive, Halifax, Nova Scotia
Stress Management Group
Wednesdays: 3:00 pm to 4:30 pm
Mental Health Day Treatment Group Room #3102, 3rd Floor
QEII Heath Sciences Centre
Abbie J. Lane Building
5909 Veterans’ Memorial Drive, Halifax, Nova Scotia
Wellness Group
Mondays: 9:30 am to 11:30 am
Duffus Street Medical Centre
The Village at Bayers Road
7071 Bayers Road, Halifax, Nova Scotia
Acupuncture and Meditation
Wednesdays: 6:45 pm to 7:45 pm
Mental Health Outpatient Department Group Room #3047, 3rd Floor
QEII Heath Sciences Centre
Abbie J. Lane Building
5909 Veterans’ Memorial Drive, Halifax, Nova Scotia
CFQ Healing
Note: Although a referral is not required for this group, you do need to register at the Mental Health Outpatient Department reception desk (3rd Floor, Abbie J. Lane Building) the first time you attend.
Wednesdays: 4:00 pm to 5:00 pm
Gymnasium, 4th Floor
QEII Heath Sciences Centre
Abbie J. Lane Building
5909 Veterans’ Memorial Drive, Halifax, Nova Scotia
Monday, October 23, 2006
Sixteenth Annual Research Day
Biology and Environment Interactions
The day’s plenary speaker, Dr. Michael Meaney of McGill University, gave a well-received and detailed presentation on how environmental cues can influence the expression of a specific gene – in this case, the glucocorticoid receptor gene.
In his fascinating talk, Dr. Meaney outlined many years of painstaking research that has shown how maternal tactile stimulation (licking/grooming) of rat pups during the first hours of their lives has a significant effect on the level of methylation of a promoter region in the glucocorticoid receptor gene that binds the transcription factor, NGFI-A.
Dr. Meany’s presentation reminded me of a line I once read in Dr. David J. Miklowitz’s book, The Bipolar Disorder Survival Guide: “As you read on [in the book], try to think of biology and environment as interacting with each other – you’ll have an easier time making choices about treatments if you can keep these multiple causes of bipolar disorder in mind.”
I'll post more about Dr. Meaney's research at a later date.
Sunday, October 22, 2006
Wednesday, October 18, 2006
Bipolar Disorder and Employment
Tuesday, October 17, 2006
Wait Times for Mental Health Services
Wait times for appointments with each of the five Community Mental Health Teams within the Capital District Mental Health Program are posted here.
These reports state that the Standards for Mental Health Services in Nova Scotia indicate:
- urgent/rapid follow up clients should be seen within 7 days (actually 5 working days);
- semi-urgent clients should be seen within 28 days (semi-urgent is not defined in the Standards, nor is the 28-day wait time); and
- regular clients should be seen within 90 days.
Wow, with three month wait times, I'm glad that I have always been an urgent client. I wonder how one qualifies to be a 'regular client'?
Because of the unfortunate stigma associated with mental illness, I would think that those of us with enough courage to access mental health services deserve to be treated as either an urgent or a semi-urgent client - at least for the first appointment.
David Rodenhiser, a columnist with the Halifax Daily News, has written a nice opinion piece entitled: A collision course. An ailing mental-health system results in more troubled people in conflict with the law. Among numerous important issues that he addresses, Mr. Rodenhiser questions the 18-day wait times (in August 2006) for those with urgent mental-health problems as reported by Mental Health Services, Bedford/Sackville.
Mental Health Services, Bedford/Sackville
Services are available:
8:30 am to 4:30 pm
Monday and Wednesday through Friday
8:30 am to 8:00 pm on Tuesday
Location:
Cobequid Community Health Centre
Mental Health Services, Bedford-Sackville
40 Freer Lane
Lower Sackville, Nova Scotia B4C 0A2
For more information visit Mental Health Services, Bedford-Sackville.
Halifax Bipolar Support Group
Mental Health Mobile Crisis Team
Toll Free: 1-888-429-8167
This new service provides mental health crisis support to individuals of all ages. Telephone crisis support is available 20 hours per day - between 9:00 am and 5:00 am.
Mobile crisis response is available every day, between the hours of 1:00 pm and 1:00 am in Halifax, Dartmouth, and Bedford.
Click here and here for further information on the Mental Health Mobile Crisis Team.
Note: The Emergency Psychiatric Assessment Services (Nova Scotia Hospital 464-3114; QEII Health Sciences Centre 473-2043) can be also contacted for emergencies outside of the hours of 8:30 am - 4:30 pm, Monday to Friday, as well as on weekends and holidays.
Summary Information on Mental Health Services
This Blog is my attempt to possibly help rectify this dismal situation.
The Nova Scotia Division of the Canadian Mental Health Association provides a summary sheet of mental health services in the Capital Health District.
Mental Health Services Directory
Note: Six corrections to the directory can be found here. Also, the phone number for the Metro Turning Point Shelter (page 3) should be (902) 420-3282; and the phone number for Byrony House (page 3) should be (902) 429-9008.
